
Prostate cancer survivors in Angus and Fife have welcomed new research which shows how combining two types of technology can detect the disease at an earlier stage and potentially save lives.
Carey Gibb, from Angus, and David Astill, from Kirkcaldy, were both in their 50s when they were diagnosed and believe early detection is key to saving lives.
They praise the new research from the University of Dundee which found that using ultrasound and MRI Technology together can locate prostate cancer earlier.
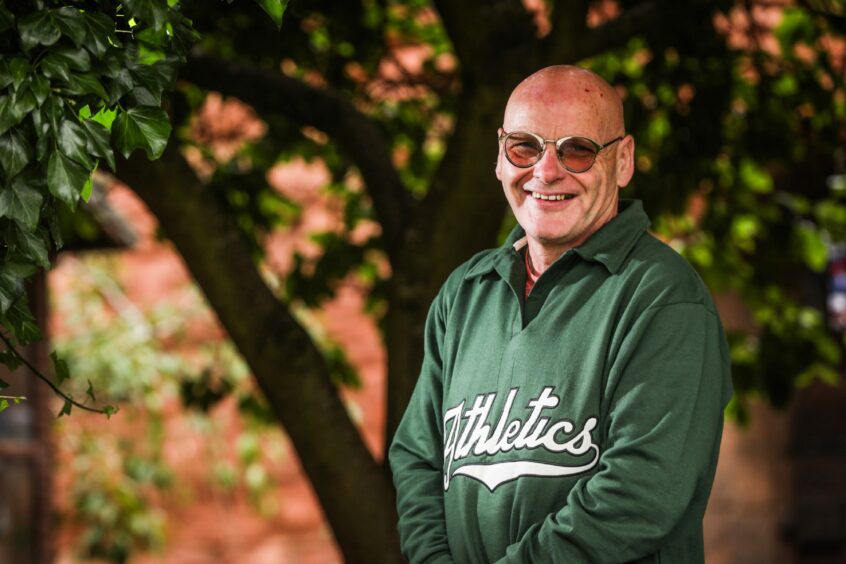
Carey, who lives in Arbroath, was diagnosed in 2017 at the age of 56.
“I was going to the toilet more during the night and there would be times I couldn’t hold it – I had this immediate need and had to use the toilet straight away.
“I went to the doctors and explained what had been happening and he gave me a PSA blood test.”
A PSA test measures the amount of prostate specific antigen (PSA) in your blood and a raised PSA level may suggest you have a problem with your prostate, but not necessarily cancer.
He continued: “The test came back which showed I had a higher level and the doctor did a prostate examination and found it was irregular.”
Carey had surgery for prostate cancer
Carey was sent to Ninewells Hospital in Dundee where a biopsy was taken.
And the results showed he had prostate cancer.
He ended up having to get his prostate removed by robotic surgery.
Robotically assisted surgery is performed by a surgeon operating a robot, using keyhole technology.
Carey, who is a stonemason to trade, explained: “The cancer was stage one going into stage two.
“But it was in three pieces and it took a few biopsies.
“I had the robotic surgery in Aberdeen in January 2018 to remove my prostate.”
New prostate cancer research from Dundee could save lives
Carey, 62, who has regular check ups which have shown no signs of the cancer, welcomes the new research.
He added: “I would urge men to just go and ask for the blood test.
“You just have to do it because it you don’t, it could put your life at risk. I was lucky so anything that can find the cancer early is a great thing.
“I think this new research is brilliant and could save lives by detecting prostate cancer sooner.”
When was David diagnosed with prostate cancer?
David was diagnosed with prostate cancer six years ago when he was 59.
He had no symptoms, apart from going to the toilet a couple of times during the night fairly regularly.
The 65-year-old said: “My only symptom was night visits to the bathroom, I had no other symptoms.
“I went to see my GP about another issue. I only mentioned the night visits to him as I was going out the door.
“Thankfully, he picked up on my comment immediately.”
David’s GP recommended he have a PSA blood test which showed elevated levels and this led to biopsies.
“There were 10 samples taken and cancer was found in each one.”
Importance of the new study
The retired director of business at Adam Smith College went on to explain why the results of the new study are so important.
He said: “The MRI I had was inconclusive as to whether the cancer had broken out of the prostate.
“But if the new combined technology had been used, it would be able to show definitively if the cancer has spread into other areas or not.
“This would take away a lot of anxiety.”
In July 2017 David went on to have robotic surgery at the Western General in Edinburgh which removed the prostate and 19 lymph nodes.
He said combining the new technology would also have been able to confirm how advanced his cancer was.
“When I was diagnosed with my biopsies I was told I was stage one.
“But when I had my MRI they queried whether there had been cancer breaking out from the prostate, so they said it could be stage two.
“Then after the surgery, I was told it was stage 3b cancer – stage three is split between A and B.”
David said it was an anxious time to have to wait before it could be confirmed what stage the cancer was at.
“So the earlier the accurate information comes from this new technique the better.”
David welcomes the new research
David, who has regular blood tests which have shown the cancer to be undetectable, welcomes the new study from the University of Dundee.
He said: “The research is absolutely excellent because it is actually improving the precision by which a biopsy can be taken.
“This then leads to an accurate result.”
How many men in Scotland have prostate cancer?
According to figures from Public Health Scotland, published in December 2022, there were 3,543 men diagnosed with Prostate Cancer in Scotland from July 2020 to June 2021.
While data from NHS Scotland reveals around 3,400 men are diagnosed with prostate cancer every year.
Prostate cancer mainly affects men over 50 and the risk increases with age.
What were the findings of the prostate cancer Dundee research?
The study was led by Ghulam Nabi, Professor of Surgical Uro-oncology at the University of Dundee’s School of Medicine.
It found the new US/MRI fusion targeted biopsy detected more clinically significant prostate cancer lesions than existing detection methods.
Currently the most common tests to diagnose prostate cancer are a PSA blood test, digital rectal examination, MRI scans, and biopsy.
But it has been shown that MRI scans aren’t always able to give a definitive answer.
And ultrasound has similar issues.
Professor Nabi said: “As with all cancers, the earlier that prostate cancer is detected then the more likely that a patient will have a more positive outcome.
“Anything that speeds up diagnosis is therefore potentially lifesaving.
“One of the problems with current diagnostic methods is they are sometimes unable to identify which cancers are benign and which need treatment.
“Our results suggest if this new approach was given to men routinely then prostate cancers would be detected earlier.
“Lives would be then saved, and unnecessary surgeries avoided.”
What did the clinical trial show?
The research was published recently in the journal Radiology.
It tested the accuracy of the new combined US/MRI fusion biopsy with existing methods.
In a clinical trial, 413 participants with suspicious prostate lesions were given either systematic random prostate biopsies alone or US/MRI fusion targeted biopsies.
Significant lesions were found in 51% of cases in the former group and 63% in the latter.
This showed that combining US/MRI fusion was a more effective way of detecting prostate cancer.
The research was funded by Prostate Cancer UK, Movember and the Scottish Government’s Chief Scientist Office.
Dr Hayley Luxton is a senior research impact and intelligence manager at Prostate Cancer UK.
Dr Luxton said: “We’re excited this research adds to existing evidence showing that targeted biopsies, guided by mpMRI imaging, improve the accuracy of prostate cancer diagnoses.
“This could lead to more men with the disease living better and longer lives.
“I’m proud that Prostate Cancer UK has supported Professor Nabi’s work for over a decade.
“And I am especially pleased this vital study has taken place in Scotland, where currently 1 in 3 men with prostate cancer are diagnosed too late for a cure.”












Conversation